What to know about a black line on the nail
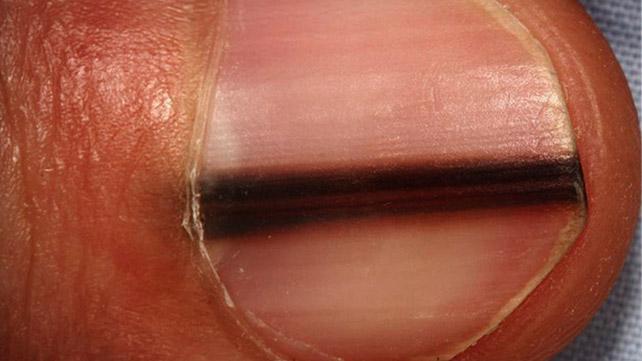
When a person has black or dark stripes running down their nails, the explanations can range from something normal through to severe, such as melanoma.
A person should not ignore changes to their nails, especially if they are painful, bleeding, and without explanation.
Fast facts on black lines on the nails:
- There are many causes of this condition, both of no concern and serious.
- Treatment depends on discovering the underlying cause.
- A person should see a doctor if they notice a change to their fingernail that cannot be explained by a trauma.

Most commonly, dark stripes down a person’s nail are due to a symptom known as linear melanonychia. According to the United Kingdom’s National Health Service, these stripes commonly occur in those of African-American descent who are age 20 and older.
Linear melanonychia is considered a normal fingernail color variation. The condition occurs when pigments in the nail known as melanocytes make excess pigment. This causes the nail beds to darken.
According to an article in the journal Podiatry Today, an estimated 50 percent of African-Americans have this condition.
Less common causes of nail melanonychia exist. These include:
- taking certain medications, such as chemotherapy drugs, beta blockers, anti-malarial drugs, or the medication azidothymidine
- HIV
- Laugier-Hunziker syndrome
- Lupus
- Peutz-Jeghers syndrome
- scleroderma
Another cause of black lines on the nails is a splinter hemorrhage, which occurs when blood vessels under the fingernail are damaged, often due to injuries, such as hitting.
More seriously, a black line or lines on the nails can indicate the presence of melanoma, a dangerous form of skin cancer.
Melanoma under a fingernail is known as subungual melanoma. One of the melanoma types is known as acral lentiginous melanoma (ALM).
According to clinical guidelines published in the Journal of Foot and Ankle Research, about half of all melanomas on the hands and feet are due to ALM.
Typically, healthy fingernails will have small vertical ridges in them, are curved downward from the nail, and do not crack or break easily. However, there are times when a person may experience black lines on the nail.
Linear melanonychia
When a person has linear melanonychia, they may see dark stripes running down the nails. They may have color variations that range from black to deep brown and gray. These lines will normally appear on 2 to 5 fingernails, but not necessarily all 10.
Subungual melanoma
When a person has subungual melanoma, they will usually notice a stripe on one fingernail only. Often, they cannot link the stripe’s appearance back to an injury.
Typically, a black stripe from subungual melanoma will darken or widen with time. Sometimes, the nail will be painful or bleed.
The pigmentation may also extend to the area where the fingernail meets the cuticle. This is known as Hutchinson’s sign, which is often an indicator of melanoma. The stripe can occur on either the fingernails or toenails.
According to the journal Podiatry Management, an estimated 40 to 55 percent of cases of subungual melanoma occur on the foot.
Splinter hemorrhage
Splinter hemorrhages appear as small black or deep-red lines and are caused by injuries to the small blood vessels under the nail beds. They usually heal on their own within a few days.
If a person has multiple splinter hemorrhages across several different nails, it could indicate an underlying condition.

The diagnostic process for dark lines under the fingernails usually starts with a persons’ medical history.
Questions a doctor may ask include:
- How long have the lines been present?
- When were you first aware of the lines?
- Have you noticed any recent changes to the lines?
- Have you had a trauma to the nails that may have caused these changes?
A doctor will also ask about medications. If a person has a history of taking blood thinners, such as warfarin or aspirin, this could explain splinter hemorrhages.
Sometimes a doctor will take a biopsy or sample of the nail area. They will send this biopsy to a pathologist, who can identify if any cancerous cells might be present.
Most causes of black lines on the nail do not require treatment. Melanoma is an exception. A doctor will usually first remove the area of melanoma as well as the skin under the fingernail.
A doctor can perform a skin graft over the fingernail to improve the finger’s appearance post-surgery.
If the melanoma had spread to the bone, a doctor might recommend amputating the finger to stop the melanoma spreading.
It is especially important to see a doctor if a person has a nail that is bleeding and painful or has changes without a known cause.
A person should see their doctor if they notice changes to the quality of the nail itself, such as thinning, cracking, or differences in the shape.
Most black lines on the fingernails and toenails are harmless. However, if a person has melanoma, the earlier the condition is diagnosed, the better their prognosis.
According to the Journal of Foot and Ankle Research, melanoma that occurs in the foot or toenail has a poorer prognosis than melanoma in other locations, as it may not always be diagnosed early.
- Dermatology
5 sourcesexpanded
- Acral lentiginous melanoma (ALM). (n.d.)
https://www.aimatmelanoma.org/melanoma-risk-factors/melanoma-in-people-of-color/acral-lentiginous-melanoma-alm/ - Bristow, I. R., de Berker, D. A. R., Acland, K. M., Turner, R. J., & Bowling, J. (2010, November 1). Clinical guidelines for the recognition of melanoma of the foot and nail unit. Journal of Foot and Ankle Research, 3, 25
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2987777/ - Morse, M. J. (2012, June). When a patient presents with longitudinal nail pigmentation. Podiatry Today, 25(6), 24–32
https://www.podiatrytoday.com/when-patient-presents-longitudinal-nail-pigmentation - Nail abnormalities. (2016, December 9)
https://www.nhs.uk/conditions/nail-problems/ - Vannuchhi, P. (2012, November–December). Melanonychia striata and the evaluation of pigmented nail streaks. Podiatry Management
http://www.podiatrym.com/cme/CMENov12.pdf
